Tristan Yan
Sydney Cardiothoracic Surgeon

Sydney Cardiothoracic Surgeon

Thoracic Aortic Aneurysm
A High Index of Clinical Suspicion
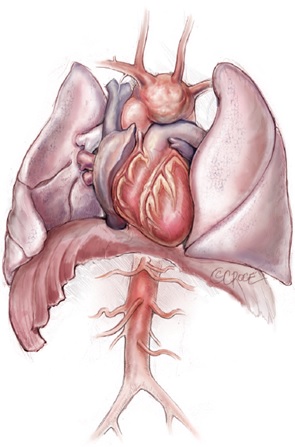
Aortic aneurysm is a common aortic pathology requiring prompt surgical intervention. The symptoms associated with an aortic aneurysm can often be subtle, including those related to aneurysm expansion (e.g. chest pain or breathlessness) and compression of adjacent structures (e.g. hoarseness or stridor). Unfortunately, many of patients may be undiagnosed or even misdiagnosed, until they present with catastrophic complications, such as acute aortic dissection, aortic rupture, cardiovascular collapse, malperfusion and/ or death. This is why ‘aneurysm’ has been perceived as the ‘Great Masquerader’ in the surgical literature (Figure 1). As the thoracic aortic aneurysm enlarges, the aortic wall tension increases. If the blood pressure is too high, the aortic aneurysm may burst or dissect, which often leads to death. We, as clinicians, ought to maintain a high index of clinical suspicion for patients with a possible aortic aneurysm.

Figure 1. Thoracic Aortic Aneurysm – the ‘Great Masquerader’
Thoracic Aortic Aneurysm is a Genetic Condition
Thoracic aortic aneurysm is a genetic condition. Marfan syndrome is just the tip of the genetic iceberg. One of the simplest screening test that we do during our initial consultation is the ‘Thumb and Palm’ sign for Marfan syndrome. If the patient’s thumb can go all the way across his/her fully extended palm, it may mean that the patient’ long bones are extensive and joins are lax, a sign of connective tissue condition that may be related to Marfan syndrome.
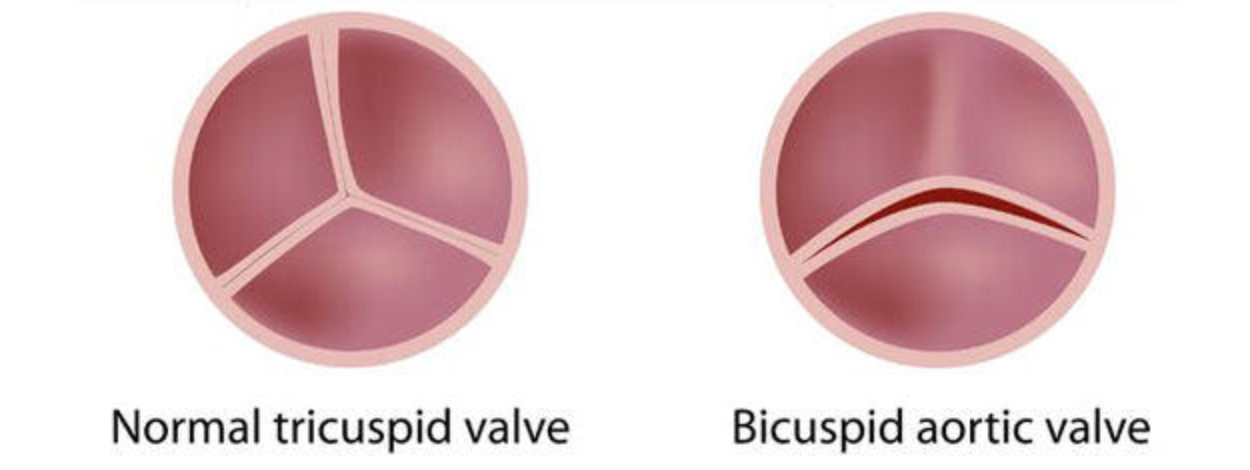
1. First-degree relatives of patients with a BAV and/or a familial form of TAA and dissection should be evaluated for the presence of a BAV and asymptomatic thoracic aortic disease.
2. All patients with a BAV should have both the aortic root and ascending thoracic aorta evaluated for evidence of aneurysm.
How to Diagnose Thoracic Aortic Aneurysm?
Initial assessment is transthoracic echocardiography to evaluate proximal aorta and valvular pathology. To visualize distal ascending aorta, aortic arch and descending thoracic aorta, computed tomography (CT) Thoracic
Aortogram is the most commonly used imaging modality for the diagnosis of TAA. It provides information regarding the size, location, and extent of the disease. The other imaging techniques include: CXR, MRI, TOE and aortography. We can perform detailed analysis, such as 3-D printing, 4-D flow MRI and Computation Fluid Dynamic Analysis to analyze aortic wall tension and sheer stress in order to monitor aortic behavior more closely (Video 2).
